Genomic Medicine: The Future of Healthcare
By: Cathrina Nauth
From head to toe, we are all different. We come in different shapes and sizes, and none of us are the same, inside or out. So why treat our bodies like we are? Modern medicine often uses a “one size fits all” approach to treat everything from the common cold to serious diseases like heart disease or cancer. However, some treatments may work better for some patients than others because of differing human genomes, which forces physicians to use a trial-and-error method to determine whether or not a particular treatment is sufficient from patient to patient. Using the wrong treatment can result in no change in the patient’s condition to a drastically negative change in the patient’s condition, often from an incorrect drug prescription. Consequently, it is necessary to tailor health care to patient differences for an individualized and effective approach. Personalized treatments will have more effectively designed drugs, allow physicians to prescribe the best treatments for each individual patient and to identify or monitor patients with a high risk for particular health implications. Studying human genomics will improve modern-day approaches to health care.
Human genomics is the study of the entire set of genes found in the human body. The human genome itself consists of a sequence of approximately three billion component parts known as nucleotides. The four nucleotide bases—adenine, guanine, cytosine and thymine—combine in pairs which code for the sequence of amino acids the body uses to build proteins. A combination of three nucleotides will code for one of twenty amino acids. For example, GCA codes for the amino acid alanine. Chains of amino acids are then linked together to form proteins, which contribute to structure, function and regulation of body tissues and organs, in addition to features such as behavior, learning and predisposition to disease. A segment of one DNA molecule that codes for one specific protein is known as a gene. There are approximately 20,000 to 25,000 protein coding genes altogether. This entire structure is referred to as the human genome.
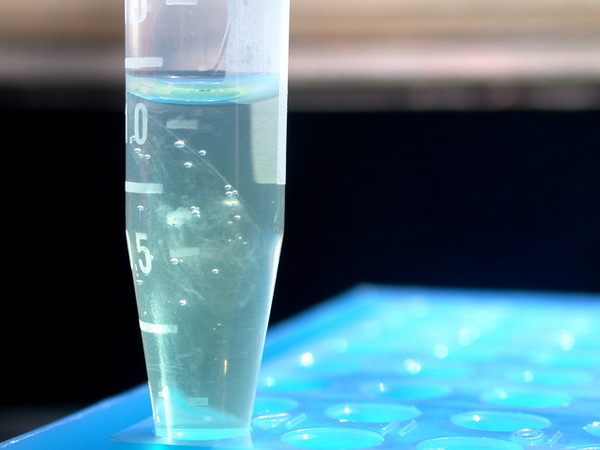
Analyzing and understanding the human genome is crucial to modern healthcare. Think of it like taking a car to a mechanic shop. One would expect the mechanic to know about every part of the car in order to determine the problem and to be able to fix it properly. Healthcare works the same way. People expect physicians to know as much as possible of their individual genomes in order to properly diagnose and treat them, for a patient’s genetic makeup is the key to their care. However, this would be physically impossible without holding ample knowledge of that individual’s genome, or “genetic blueprint.” For this reason, the Human Genome Project (HGP) was founded, which aimed to put the three billion pairs that make up the human DNA into a proper sequence and to identify every protein coding gene written within these molecules. In order to sequence the genome, the HGP’s primary method was to use map-based, or BAC-based sequencing. In this process, human DNA was fragmented into large pieces and cloned into bacteria, which would replicate the DNA so that it would be prepared in quantities large enough for sequencing. Each BAC clone was “mapped” to determine where the DNA in the clone came from in the human genome. This allowed scientists to determine the precise location of the DNA letters. For sequencing, the BAC clone is cut into a smaller fragments known as subclones. A “sequencing reaction” is then performed and the products are put into a sequencing machine, known as a sequencer, and then a computer assembles the sequences in order to enable them to represent DNA in the clone.
With the DNA sequenced, and the human genome identified, personalized medicine can become possible. Personalized medicine, commonly known as genomic medicine, is a way to use the human genome to customize medical care based on individual’s unique genetic makeup and gene expression patterns. Genomic medicine allows for targeted therapies because unfortunately, the “one size fits all” pharmaceutical model is not very effective at all times, for most drugs produce a spectrum of responses in various recipients. Targeted therapies will allow physicians the ability give particular drugs to those of whom it is effective, and avoid giving it to those of who it would be of no help. Targeted therapies also allows for the revitalization of older drugs that may have been disregarded because it only cured a small population at the time it was first used, but would be beneficial for a person right now.
In addition to the genome-guided treatments in patients with complex diseases through targeted therapies, genomic medicine can be beneficial and gaining a momentum in other areas. For one, genomic medicine can assist in the risk assessment of healthy individuals. For example, according to the National Cancer Institute at the National Institutes of Health, women with the BRCA gene mutation have a 40% chance of developing breast cancer within the next ten years. By analyzing the genome and shedding light on this mutation, women can take preventive measures such as receiving tamoxifen treatments or having an oophorectomy. Besides risk assessment, genome analysis can help in early detection, such as individuals with mutations for colon cancer, who would benefit from earlier and more frequent screenings to detect in its earlier stages. Aside from risk assessment and early detection, genomic analysis can assist in diagnosis and prognosis. For example, in certain types of heart diseases, any detection of particular gene mutations can lead to the diagnosis and early treatment to prevent sudden cardiac death before symptoms occur. Furthermore, by identifying individual gene differences, better medications and proper dosages can be selected for the best results.
Genomic medicine is expected to have an immense impact on healthcare in the upcoming years, for genomic medicine is gaining momentum across a continuum of clinical practices including everything from dermatology, anesthesiology, and endocrinology to pathology, cardiology and even psychiatry. For example, newly discovered results from genome-scale genetic studies of schizophrenia and autism suggest specific areas of neural function as possible sources of disease risk. On the other hand, genomic medicine can help in areas like cardiology, for some recent studies from the American College of Cardiology Foundation have shown that specific DNA variants and genes known as LPA, CXADR and APOE are genetic markers for becoming susceptible to coronary artery disease and even sudden cardiac death. To look at it as a whole, genomic medicine can assist in copious amounts of specialties. In fact, there are very few specialties where knowing the human genome would not assist, proving its profound impact on the future of healthcare.
After analyzing the various aspects and profound impact genomic medicine would be able to make in healthcare, it is necessary to realize the key enablers that would allow for its integration into healthcare. For one, genomic literacy is important. As of right now, many people are not able to interpret the actual information, for it is very complex. Even practitioners and specialists, who are enthusiastic about the idea, have a difficult time understanding genomic information and are not prepared to deal with this in their practices. Pressing on the idea of genomic literacy is very important for this change to occur. Another enabler would have to be along the lines of securing privacy. With one’s entire genome sequence, it is not hard for the government to get a hold of the results and use it against people. For example, genome sequencing could affect one’s insurance negatively. If there are specific mutations (even if they are not deadly, or only account for a small percentage chance of acquiring a particular disease), it may affect an individual’s ability to acquire life, long-term care, or disability insurance. It could also work against an individual if their employer denied them specific opportunities after learning the results of their genome sequencing. Another enabler would have to be funding. Genomic medicine can be costly. However, individuals need to look at the big picture. Evidence-based medicines may or may not help. Also, if they do help patients, they may not always be effective. They may be sufficient in the short-run, however, it may be an improper treatment to the disease, and continuous forms of that treatment will be needed, costing a great amount, also. This would be where genomics plays a major role, for it would be able to direct the physicians to the correct targeted therapy necessary for the disease, rather than working through previous experiences and trial and error. After these implications are dealt with, genomic medicine would be easily integrated into healthcare.
All that is left to do now is in our hands. Analyzation of genomic medicine demonstrates and proves its promising future in healthcare. Fortunately, genomic medicine is already being used to radically alter healthcare today, despite its critics, for some cases of chronic diseases. According to Xi Lin’s publication on Applications of Targeted Gene Capture and Next-Generation Sequencing Technologies, a few years ago, it cost about $10,000 to have an individual’s genome sequenced. Today, with current technologies such as Illumina’s Genome Analyzer, the cost is closer to $1000. With more and more technology, having one’s genome sequenced can become more affordable and lives can be prolonged and saved. With that being said, we are halfway there. We just need to recognize the value of medical innovation. With the proper resources, the scientific community can make this possible. Remember, the future is now, and it is in our hands. We just have to make the leap.

