HIV: Beginnings and Ends
By Justin Dumrongkulraksa
When most people think of medicine they imagine a surgeon or primary care doctor, but medicine is actually a multidisciplinary field. Every treatment used by a physician began with someone like an anthropologist or historian who raised the important questions inspiring researchers in labs. Given the vast amount of resources and manpower invested in HIV research, it begs the question as to why HIV has such a shrouded origin and difficult treatment, until now. Researchers have finally traced the origin of HIV and have made breakthroughs on the potential treatment of this pandemic.
HIV has infected nearly seventy-five million people, and it garnered much public attention when it arrived in the United States in 1981 amongst the homosexual population. These men were dying of rare opportunistic infections unheard of in people with healthy immune system. In 1982, scientists began using the term AIDS for these cases and in 1983, HIV was discovered to be the agent responsible for AIDS. Isolation of HIV, however, revealed the disease had already been established in heterosexual populations of central and eastern Africa. By the end of 1980s, the genetic diversity of HIV-1 group M in the Democratic Republic of Congo was greater and more complex than that in the rest of the world. HIV is divided into HIV-1 and HIV-2 and while are transmitted via sexual contact, HIV-1 is more easily transmitted and accounts for the majority of HIV cases today. The strains of HIV-1 are then broken into groups with the major group, Group M, and the outlier group, Group O. Group M is the group of HIV strains responsible for the current HIV pandemic, but how this group of viruses became so widespread was a mystery until now.
Using the latest phylogenic techniques, researchers from Oxford University were able to statistically estimate the origin of the HIV pandemic by comparing the HIV genome from different sample regions. HIV-1 group M pandemic ignited in Kinshasa, Democratic Republic of the Congo, around the early 1920s and its expansion into central Africa was dependent upon an active transportation network, particularly railways, which connected the country’s main population centers to other regions of sub-Saharan Africa. The researchers noted that social changes surrounding African independence in the 1960s likely led to the spread of infection from small, isolated populations to larger populations, eventually leading to a worldwide pandemic. Other contributing factors include a high number of sex workers in the 1960s, as well as public health campaigns against other diseases that led to the unsafe use of contaminated needles.
Understanding how a disease spread is one of the first steps to designing effective prevention, treatment, and cure. Unfortunately, the nature of HIV makes the curing part much more difficult than prevention or treatment. Since HIV was determined to be sexually transmitted, condoms have become the primary prophylaxis. Condoms are 90- 95% effective when used consistently, and though imperfect, they provide substantial protection against HIV infection. Vaccines are problematic because HIV has specific molecular adaptations that enable it to thwart innate and adaptive immune mechanisms. These include massive replication, high mutation rates, genetic malleability, and functional plasticity which promote rapid evolution, and the establishment of latency. Thus, not only can the virus hide from the immune system, but once detected it is well equipped to bypass bodily defenses or mutate into an unrecognized form. This combination of factors is why it is so difficult to manufacture a vaccine: high mutation rates render a vaccine ultimately ineffective.
Antiretroviral treatment (ART) is the most common form of HIV treatment used to treat the symptoms, but several recent news stories claimed these drugs could actually eradicate HIV in infected infants. In March 2013, Medical News Today reported that researchers from Johns Hopkins Children’s Center, the University of Mississippi Medical Center, and the University of Massachusetts Medical School had “functionally cured” a 2-year-old infant born with HIV, thus the child had no detectable signs of viral replication in her blood after antiretroviral therapy
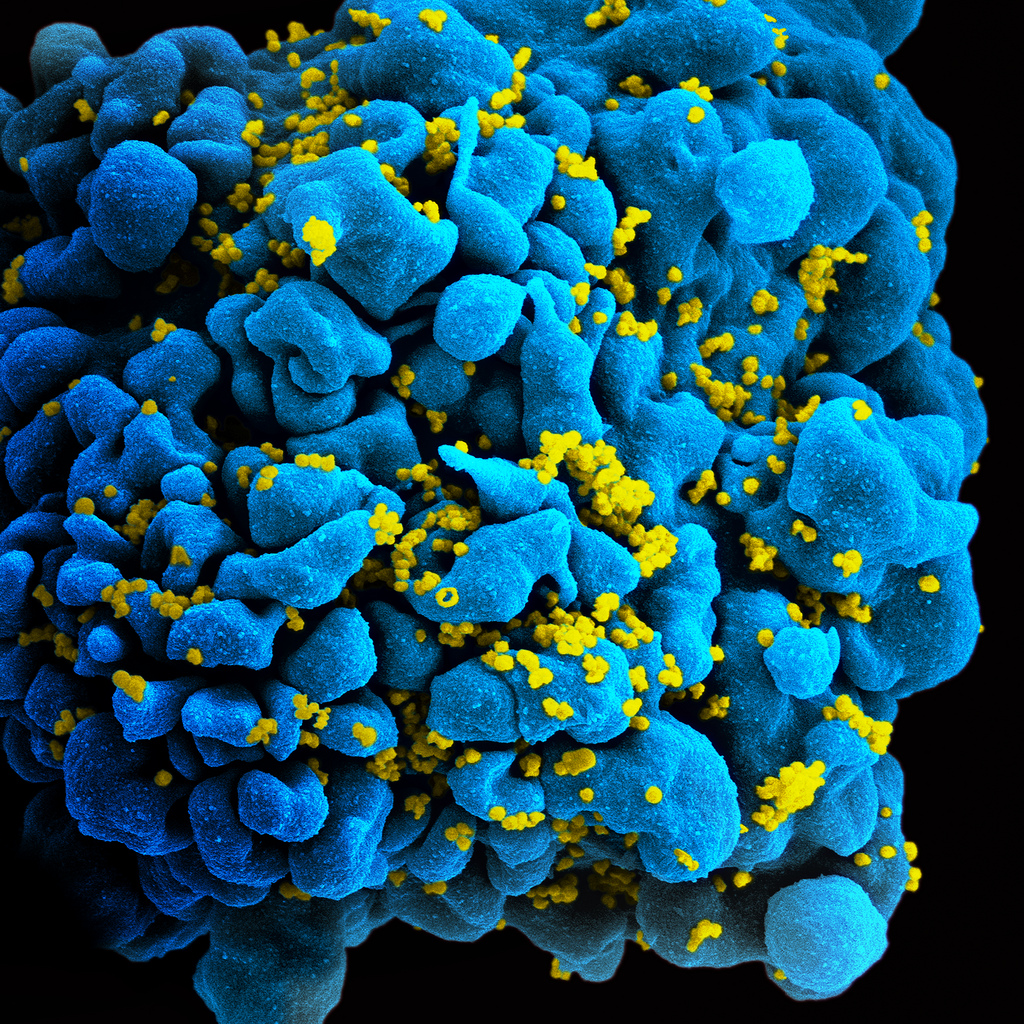
(ART) had ceased. Eighteen months after the child had stopped receiving ART there were still no signs of viral replication, which the researchers claimed provided “compelling evidence” that if an HIV-positive child is treated with ART within the first hours or days of infection, viral remission is achievable. On July 2014, however, during a routine clinical care visit, (the child’s) doctors found detectable levels of HIV in the child’s blood. Later it was discovered that the child’s parents had not keep (kept) up her drug regime. In addition to detecting the virus, there was also indication the virus was actively replicating given the reduced levels of the virus’s host: memory immune cells known as CD4+ T cells.
CD4+ T cells are responsible for fighting foreign invaders that the body has come across previously. Early in HIV infection, viral DNA occupies these memory cells and lies dormant in them. When these memory cells awaken as part of an immune response to another pathogen, however, the HIV DNA is activated and viral replication is triggered. ART only fights HIV when it is actively replicating and is unable to stop it when it is dormant in the memory cells. But three recent HIV rebound cases indicate that an HIV cure may lie in eradicating infected memory cells.
A new case report published in The Lancet, reveals that a baby born in 2009 believed to have been cured of HIV in Milan, Italy, now has detectable levels of the virus in his blood. Even when the HIV virus was undetectable in the child’s blood, his immune system continued to respond as if it was fighting the infection making this case different from the Mississippi baby who had no detectable immune response. The researchers concluded, however, that this case and that of the Mississippi baby indicate that although antiretroviral drugs are effective in reducing HIV morbidity and mortality, they are ineffective in eliminating viral reservoirs and are thus unable to eradicate HIV.
The key to eradicating HIV might lie in improving detection of latent infected immune cells. Dr. Silicano explains that reservoirs of infected memory cells only occur in a few out of millions of
immune cells, and only around 2% of these cells circulate in the blood at any given time. Thus it is challenging to test for this even using larger blood samples. The presence of infected memory cells may indicate the length of time a patent is likely to be in remission. If a patient has other infections, however, this may activate the memory T cells and trigger the HIV infection out of latency. It is possible a patient may never experience a relapse, but he or she is at risk even if they only possess one infected memory T cell.
“…what these cases underscore is the ability of even a few such cells to rekindle infection after prolonged remission.” –Dr. Robert Silicano, Howard Hughes Medical Institute
Researchers made a breakthrough in pinpointing the origin of HIV, but the search for a cure is still on. Medicine is more than just treating patients. Medicine relies on discoveries such as the Mississippi and Milan cases to design the safest most effective treatments. And research is very multidisciplinary. The pinpointing of the origin of HIV required understanding of the socio-political climate of the early twentieth century Congo to determine how HIV was able to become a pandemic. It also required a zoological understanding to know how SIV (HIV) could be transmitted to humans to become HIV. Now, as we continue to find a cure for this pandemic, we need every perspective we can get to finally eradicate this elusive disease.

