APPENDECTOMY VS. MEDICATION THERAPY

 BY RALEIGH DURAN – For many people, the initiation of right lower quadrant pain and some vomiting elicits immediate dread over a trip to the Emergency Room and possibly the Operating Room. Appendicitis is commonly cited as the major fear for patients with abdominal pain, most likely due to the horror stories of ruptured appendices and the threat of death by sepsis. Given the fear over appendicitis, many people even request the removal of their appendix during other routine abdominal surgeries, just for the peace of mind. Traditionally, there was no dispute over surgical techniques for appendicitis, and surgeons often noted that an appendectomy was the “bread and butter” of surgery, an estimated fifteen minutes in the Operating Room with patients lining up for the operation. Up until recently, little was known about the functions of the appendix, and many had written off this “random intestinal appendage” as a vestigial, or no longer necessary, organ that did not serve a purpose for the modern day human body. It would have seemed outlandish to suggest that a patient could go home on an antibiotic for their appendicitis, but current research suggests otherwise.
BY RALEIGH DURAN – For many people, the initiation of right lower quadrant pain and some vomiting elicits immediate dread over a trip to the Emergency Room and possibly the Operating Room. Appendicitis is commonly cited as the major fear for patients with abdominal pain, most likely due to the horror stories of ruptured appendices and the threat of death by sepsis. Given the fear over appendicitis, many people even request the removal of their appendix during other routine abdominal surgeries, just for the peace of mind. Traditionally, there was no dispute over surgical techniques for appendicitis, and surgeons often noted that an appendectomy was the “bread and butter” of surgery, an estimated fifteen minutes in the Operating Room with patients lining up for the operation. Up until recently, little was known about the functions of the appendix, and many had written off this “random intestinal appendage” as a vestigial, or no longer necessary, organ that did not serve a purpose for the modern day human body. It would have seemed outlandish to suggest that a patient could go home on an antibiotic for their appendicitis, but current research suggests otherwise.
With the more recent interest in the gut microbiome, scientists are learning more and more about the enigma, that is, our gastrointestinal tract. With numerous complexities and disorders, it seemed possible that various portions of the GI tract could be overlooked, and despite copious research, a complete understanding is still unlikely. At this point, physicians and scientists alike understand that the GI tract, particularly the intestines, relies on bacteria for proper digestion, absorption and excretion. Funds have been poured into researching the necessary and symbiotic relationship between our intestines and the bacteria that they house, and more recently we have learned that the appendix may play a larger role in this than previously thought.
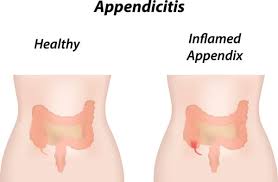
Gathering the information, research data and current understanding of the gut microbiome, the assumption at this point is that the appendix, a bacteria containing sac on the outskirts of the iluem, is necessary to maintain equilibrium with the gut bacteria. When the balance is off, the appendix can seemingly disperse more bacteria into the environment in order the aid digestive processes, and when bacteria counts are too high, the appendix can draw bacteria back in for later use. This function has become more evident with updated research methods, and clinicians are now considering the possibility of treating appendicitis with antibiotics alone.

Surgical Removal of Inflamed Appendix
Observing the correlation between appendectomy patients and increased risk for autoimmune disease, researchers began to expect and hypothesize that the appendix was involved in the relationship between the autoimmune and gastrointestinal systems. Over time, physicians and surgeons began to notice that appendectomy patients were more inclined to develop autoimmune disorder, running the gamut from mundane seasonal allergies all the way to the neurodegenerative disorder, multiple sclerosis. A long term study performed in China revealed that patients status post appendectomy were more likely to develop rheumatoid arthritis, an autoimmune disorder, when compared five years later with patients who had not received an appendectomy. This noticeable relationship, coupled with research data to suggest some relevance of the organ later prompted more and more research into the necessity of surgical methods to treat appendicitis, and began the exploration of antibiotic therapy.
Appendicitis is the inflammation of the appendix, likely caused by bacteria or other infectious material. Generally, physicians will treat an infection with an antibiotic, and the same principles were applied when tackling non-surgical techniques for appendicitis. In a randomized clinical, results were promising that there may be a future in antibiotic therapy for appendicitis. Studies are now suggesting that there are fewer immediate complications with antibiotics versus surgery, with a decreased likelihood of infection, abscess or other operative risks. In the trial, patients were diagnosed with appendicitis by CT scan of the abdomen, and were placed into two groups, either the appendectomy group or antibiotic treatment, Levaquin, Flagyl and IV Invanz. Groups were assigned a one year follow-up period in which the clinicians would evaluate the results. Of the 256 patients that were assigned to the antibiotic group, 186 of them did not require surgery and were successfully treated with the antibiotic course. Although 70 patient did require appendectomy in that first year, the results are promising that the future may steer clear of the operating room. With many of these trials still in their initial stages, future studies could begin to experiment with the types and combinations of antibiotics, their dosages and how they are transmitted to the patient. As medicine continues to progress and research is applied, there is hope that one day there will be a treatment option with proven efficacy that physicians can apply for the betterment of the patient.
