The leara scholarship: written winner
The following submission won the written portion of the Leara Scholarship.
YEONGSEO SON — In the western world and more developed countries, tuberculosis (TB) is rarely in the headlines. It’s considered ancient, practically eradicated. Yet, this deadly sickness is the world’s most leading infectious disease after Covid-19. It ranks higher than HIV or malaria and kills more people each year than both of those diseases combined. Caused by the bacterium Mycobacterium tuberculosis, the infection consumes the patients’ lungs, destroying healthy tissues and creating cavities. The chest hole fills with fluid, and the patient drowns, gradually, from the inside.
TB has coexisted with human beings for a long time. Evolving and mutating alongside us, this bacteria has survived over 70,000 years of history. Known to us as tuberculosis, the disease went by many other names. In Ancient Greece, TB was well known and named Phthisis by Hippocrates, who accurately delineated its symptoms and the characteristic tubercular lung lesions. In the Middle Ages, TB was widely called “king’s evil.” In the 18th century, TB was the “white plague,” which slaughtered a third of English tradesmen and employees. One hundred years later, TB became “Captain of All These Men of Death” as it ravaged Europe and North America, killing one in four men.
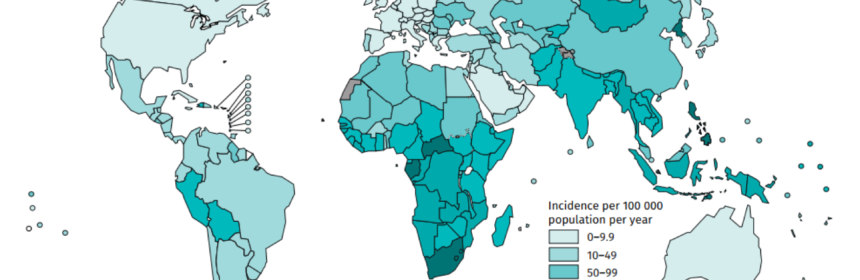
Although civilization advanced and technology exponentially evolved in recent decades, TB is very much present and rampant across the globe. Each year, including in 2020, tuberculosis kills 1.5 million people. An estimated 10 million people fell ill with the disease in the year 2020 alone. 86% of new TB cases occurred in 30 high TB burden countries. Eight countries accounted for two-thirds of the total: India, China, Indonesia, Philippines, Pakistan, Nigeria, Bangladesh, and South Africa. Funding in these low and middle-income countries, despite the desperate need for monetary support to combat TB, falls far short. The World Health Organization (WHO) estimates a $3.5 billion funding shortfall for TB control efforts. That gap could further expand in the next few years.
Because of how tuberculosis spreads, TB has always been stigmatized. Like Covid-19, TB is mainly transmitted through the air. When an infected person coughs, speaks, or sings, they may transmit the bacteria to those nearby. Because of TB’s infectious nature, the people most likely to
be affected are people physically closest to the patient, such as their family members, friends, coworkers, and schoolmates. This phenomenon — easily explained through science — often led tuberculosis to be connected with a “family curse” or “witchcraft” in some cultures. TB has also
been heavily stigmatized due to its association with social marginalization, drug and alcohol misuse, homelessness, and HIV. This stigmatization can oftentimes lead to delayed diagnosis and further contribute to the pandemic.
TB is also tricky to contain because even people who can’t develop symptoms can still infect others. In fact, one-third of the world’s population is estimated to carry “latent tuberculosis” where TB resides in a body without harming the host. Another factor is the need for long-term treatment. Effectively treating an active TB disease requires daily medication for six to nine months. The medication is usually a combination of antibiotics including rifampin, pyrazinamide, and ethambutol that can kill the bacteria and slow its growth. Although patients may feel better only after a few weeks of taking the drugs, continuing the treatment is crucial to prevent recurring tuberculosis and the development of a drug-resistant TB strain.
Multidrug-resistant tuberculosis, a massive obstacle to eradicating TB across the globe, is caused by an organism that is resistant to at least isoniazid and rifampin, the two most powerful TB drugs that are used to treat patients with TB disease. Along with patients not taking their TB medicine regularly, multidrug-resistant TB can occur when patients redevelop TB after a past infection or come from areas of the world where drug-resistant TB is common. Multidrug-resistant TB makes it much harder for low and middle-income countries that cannot afford these medications or wide testing to contain the spread of tuberculosis. And it makes it difficult to completely eradicate tuberculosis across the globe.
According to the CDC, a vaccine — known as Bacille Calmette-Guérin (BCG) — is available to prevent tuberculosis. Because of its wide success variability and limitations, only countries burdened with TB cases are advised to administer BCG. The vaccine, made almost a century ago in the 1920s, is only recommended for children (never adults) living with someone with TB who cannot take the antibiotics required to treat the infection or who is infected with a strain that is highly resistant to all antibiotics. The criteria are very narrow. In addition, BCG cannot prevent primary infection or reactivation of latent pulmonary infection, which is the main source of transmission in a community. Therefore, the impact of BCG vaccination on TB spread is severely limited.
Because of TB’s intricate immunological response, chronic progression, and the necessity for long-term treatment, it has always been a major health burden for the world. However, we already know how we can treat TB in poorer countries: the same method richer countries employed. A combination of antibiotics, extensive testing, and providing medications to destroy the bacteria before the patients even develop contagious symptoms could successfully contain tuberculosis. Because this method has proven to effectively contain TB in richer countries, the same procedures should be employed in the eight high TB burden countries.
Due to the Covid-19 pandemic, tuberculosis testing and treatment have decreased. With the ICU filling up with Covid-19 patients, beds and attention became unavailable for those with tuberculosis. However, diseases do not stop because of our busy schedules. Now is more time than ever to give the appropriate resources to TB burden countries so that they can combat TB effectively and fully. Peter Sands, the Executive Director of the Global Fund, said, “ The fewer people we find, test and treat, the more TB cases and deaths there will be, and the higher the risk of multidrug-resistant TB spreading worldwide,” Combating both Covid-19 and TB through investments in tools and healthcare should be a high priority to fight these airborne epidemics before their mutations far outpace us.
Photography Source: https://communitymedicine4all.com/2021/10/17/covid-19-causes-increase-in-tuberculosis-deaths-global-tb-report-2021/
